
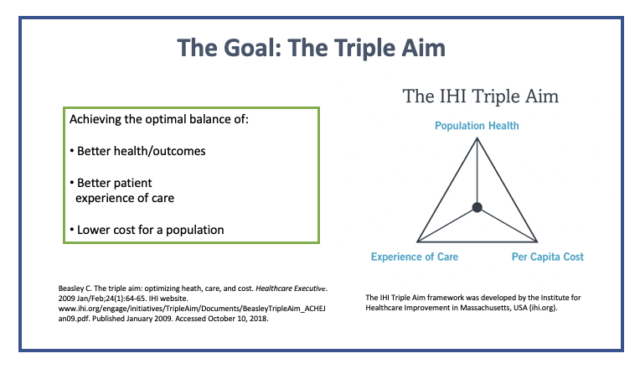
This means that as a result of an intervention, the person’s illness improves and the health of the individual increases. In the true definition, quality of care relates to clinical outcomes. Quality of care can be defined in several different ways and by different individuals. ‘In addition to the above, I would include improving the lives of the providers, especially when it relates to the areas of resilience, burnout, and suicide.’ As a result, the overall experience for the patient is less than optimal and the quality of care and the health of the patient suffer. With all these interventions, the person can be at risk for harm arising from additional testing, procedures, and medications or even invasive interventions. When a false-positive result occurs, the patient is subjected to additional tests, procedures, or even surgery to make a definitive diagnosis. Also, when unnecessary tests are done, there is a chance for what is called a “false-positive” result, meaning that the test appears abnormal when the individual does not actually have a problem. For a nonacute illness, going to an ER exposes the individual to (often times) more testing that is unnecessary and, thereby, contributes to unnecessary expense for the patient as well as the company that insures the individual. When this happens, the individual might decide to go the emergency room or to a walk-in clinic (urgent care center). This alone affects the quality of care because health care is postponed, and during this time, the condition might worsen. In certain areas of the country, it might be as long as several weeks to more than 1 month to get an appointment. Think about how long you (the reader) would want to wait to get an appointment. Access to care is often times the first challenge for a potential patient, and when it comes to outpatient care, the wait times to see a physician or to have tests or procedures completed is certainly too long. As health care providers, we have to pay attention to the experience the individuals have when engaging with all parts of the health care system. So let us first look at the patient experience, which often times is not optimal. In addition to the above, I would include improving the lives of the providers, especially when it relates to the areas of resilience, burnout, and suicide. The focal points are improving patient experience, including the quality of care and patient satisfaction improving the health of populations and reducing the per capita cost of health care. In years past, the Institute for Healthcare Improvement coined the term Triple Aim, which describes an approach to optimize health system performance. When it comes to the delivery of health care, we as providers need to be cognizant of many things which do not necessarily have to do with the actual administration of the clinical care but are, nonetheless, just as important.


 0 kommentar(er)
0 kommentar(er)
